Palantir positions itself as a data harmonizer, integrator, and analytics facilitator, yet its National Health Service (NHS) detractors label it a data thief. The current barrage of recycled criticism surrounding the company is short sighted, when really, Palantir is being scapegoated for a decade of poor NHS leadership on nurturing a data driven culture.
Now, the NHS Transformation Directorate (a merger between the former NHS Digital, NHSX, and NHS England) is spending inordinate amounts of time defending its decision to exploit the effective partnership it forged with Palantir through the pandemic.
One upcoming ‘open’ contract, yet to be run, must rank among the most controversial in the history of NHS technology procurement:
- A five-year relationship (with an option to extend by a further 2 years) worth £360m, to co-create a national data analytics platform, aka Federated Data Platform (FDP). This will enable analysis of disparate data streams from across the 42 newly established local Integrated Care Systems (ICSs).
Three key issues underpin the hotly debated and at times mis-interpreted discourse:
- Outward behaviour has had the rumour mill running at an all time high that Palantir and NHS leaders have already jointly decided the structure and running of the FDP, so that the open tender is no more than a rubber-stamping exercise, to camouflage the award of the biggest chunk to Palantir. This also includes the recruitment of two former NHS England executives who had been working closely with Palantir through the pandemic;
- No NHS-wide debate has been held to champion this next chapter, or reassure frontline teams on data sharing and privacy-by-design. Contrary to general perception, we’re told that the FDP is not intended to directly support patients’ care. It will reportedly initially be used for the national management of vaccines and immunisation programmes, population health, elective waiting lists, and meds & equipment supply chains;
- Yet, relationships are further strained when we’re to believe that shared care records, which the vast majority of ICSs now have created in some form, will feed into the FDP. Not everything adds up, and key stakeholders rightly expect transparency;
- Yet, relationships are further strained when we’re to believe that shared care records, which the vast majority of ICSs now have created in some form, will feed into the FDP. Not everything adds up, and key stakeholders rightly expect transparency;
- The company’s heritage in classified security and military-related contracts.
So much so that the release of the tender has been delayed twice so far.
Blinkered NHS Leadership
Perhaps part of the problem here lies in the drive by NHS leaders to accelerate at scale and pace. They have a legacy of spectacular failure in public, patient-advocacy, GP, and provider engagement over data sharing, ownership, and privacy.
That US providers continue to renew Palantir contracts seems to offer no reassurance on issues such as trust and data privacy. If anything, this further stokes the debate on the higher likelihood of the English model ‘descending’ towards privatised healthcare – in a culture steeped in free at the point of care, any mention of patients paying for at least some of their healthcare sparks outright fury. And yet the reality is that the self-payment model has been gaining traction among those unwilling to sit out delays of several years before being offered intervention.

There is a huge spectrum of digitally enabled transformation across the NHS. The successful stories emanate from strong local leadership teams. This in itself represents another oddity within NHS policy here : When it suits, frontline leaders are offered match funding for tech innovation and advised that ‘local knows best”; in other instances, such as with this FDP, a top down model is all but imposed.
Drowning in Data Yet Low Population Health Insight
We know that the ICSs and their aligned Boards have multiple challenges ahead to ensure on par digital maturity, while still grappling with paper-based settings and EPR deficits (a mandate has recently been set to close this deficit).
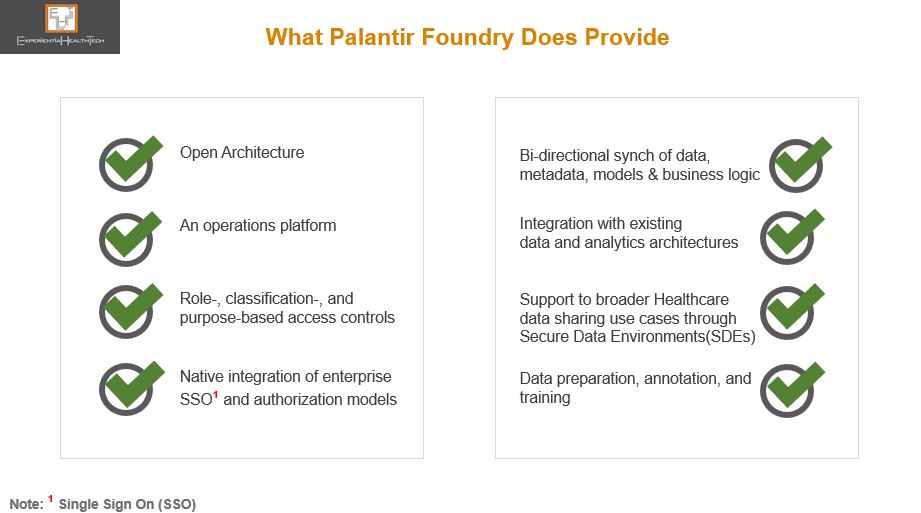
The NHS needs and wants much of what Palantir has to offer: a federated setting with strong governance foundations, interoperability, model-agnostic methods, open architecture, operational & decision intelligence, AI-on-the-fly, AI for IoT and Edge, “co-create once and repurpose”, and vertical platforms.
Most recently, through The London Medical Imaging & AI Centre for Value Based Healthcare, NHS leaders had a golden opportunity to create a wider coalition of the willing among frontline teams, to embrace a federated learning model. That hasn’t happened, with the result that this apparent leapfrog into a longer term and more consequential relationship is drawing such criticism and alarm.
But there is a clear line between both these projects: in the Value Based Care initiative, although tech companies were clearly involved, NHS Digital was in the driving seat. In this FDP initiative, the feeling is that these same leaders are handing over the crown jewels of NHS rich data to Palantir.
The justification for the tender is that the skills needed to build and manage such a platform go way beyond the collective capability of the NHS frontline, at a time of its greatest operational challenge.
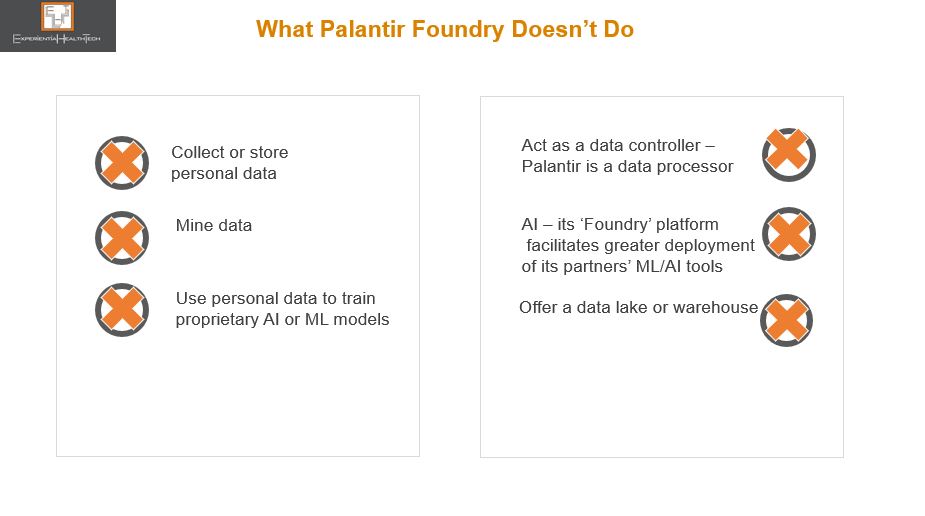
While there are clinical and IT leaders who support this move, the drive to embed this nationally is still facing strong resistance. Not to over-simplify the tensions here, it’s worth busting some myths over Palantir:
Palantir Takes Up Mentoring
Palantir has clearly worked its successful pandemic relationship with the NHS to good effect. That approach too has been criticised. But let’s face it, this is no different a tactic from other vendors over the years, including many of those that stood up solutions for free through COVID-19. Equally, many vendors have over the years sought my advice on which among the NHS England/NHS Digital/ NHSX leaders they should woo, to embed their respective tech philosophy.
Palantir has also stepped in to reassure on what to expect, should it win the largest part of the FDP work. But much of the language used is elusive to many frontline teams.
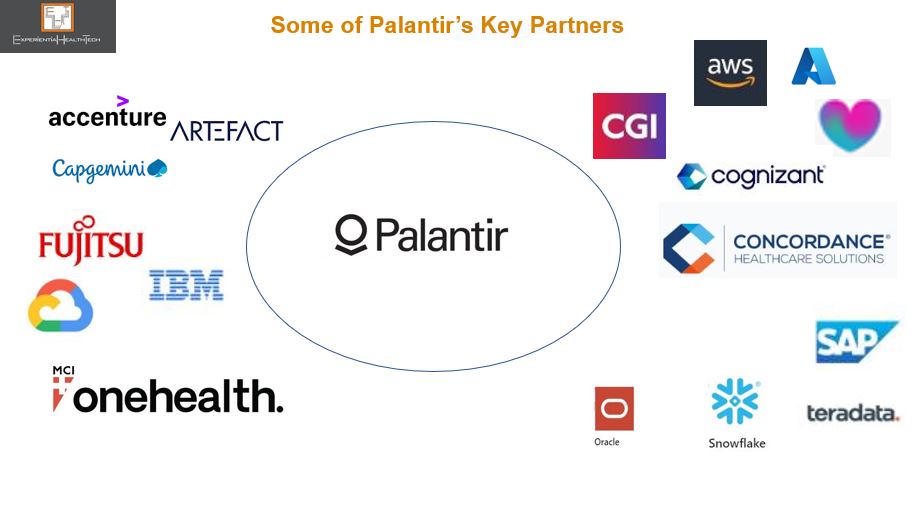
The NHS Transformation Directorate may plough on and coronate Palantir, offering the 3 other related FDP tender parts to other bidders – note that the names in the running are not mainstream to the NHS. One of these vendors has confirmed its intention to submit a bid as part of a consortium.
This is a further irony given the range of high calibre partners signing up to work with Palantir in general, many of which independently have forged solid trusted relationships with the NHS, and which within the context of this FDP contract will have to engage with Palantir on some level.
Or, as is currently politically fashionable, we may yet see a U-turn (expensive).
There is perhaps never an optimal time to go ‘big and bold’, but this is what’s being prioritised. This is high stakes for both the NHS and Palantir.
Expect the debate to rage on, post-contract award. This expenditure carries all round high expectation on deliverables and frontline outcomes over the timelines carved out.
